Getting to a successful diagnosis of ileitis

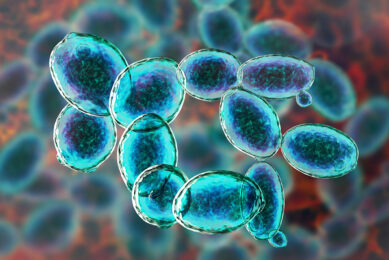
Ileitis – caused by Lawsonia intracellularis – can be a tricky disease to diagnose. The subclinical form often goes unnoticed, and several pathogens can have similar clinical presentations. This second article of the Lawsonia series covers what veterinarians can do to reach a good clinical diagnosis.
Ileitis (also known as porcine proliferative enteritis) is an important disease in the global swine industry. This makes early detection of the disease key to preventing or minimising health and performance losses. However, proper diagnosis can be complex, especially when the subclinical form is present or when multiple enteric problems or pathogens are present at the same time. A successful diagnosis approach should therefore involve several methods and steps.
Could it be ileitis?
The term ileitis represents 3 different clinical presentations. The acute and chronic forms generally manifest clinical signs, while the third form remains subclinical. Acute cases are characterised by haemorrhagic, black tarry diarrhoea and sudden death. Clinical evidence of chronic ileitis starts with the observation of loose-to-watery, grey-green diarrhoea, associated with growth retardation despite normal feed intake. Spotting sick pigs with the human eye is not enough to confirm that the problem is ileitis, as clinical signs such as diarrhoea can also be caused by other enteric pathogens.
Most difficult to diagnose is the subclinical form, where no visible signs such as diarrhoea are present. Yet the farmer or veterinarian can consider ileitis when there is reduced growth and feed efficiency or changes in batch homogeneity. Coming to a solid diagnosis relies on the combination of veterinary assessment on farm and characterisation of the gross and microscopic lesions, including detection of L. intracellularis in infected animals. To do this, the right samples are necessary. The samples the veterinarian takes are driven by the clinical picture, the foreseen diagnostic technique and the costs. PCR, for example, is quite expensive. Therefore, to reduce diagnostic costs, veterinarians can choose to run a PCR test on a pooled faeces sample (e.g. from 5 animals).
Post-mortem analysis
Necropsies (post-mortem sampling) on the farm or at the slaughterhouse are used to confirm thickening of the intestinal mucosa, the primary and most remarkable gross lesion of ileitis. The ileum can be thickened in a way that is often compared to the structure of a garden hose. In milder cases, the intestinal mucosa often resembles the longitudinal folds of cerebral cortex due to proliferation of epithelial cells and the thickness of the mucosa.
Lesions of proliferative enteritis are restricted to the intestinal epithelium. They are typically observed in the terminal ileum and cecum, and with increasing severity they may extend to include the jejunum, cecum and spiral colon. In acute cases, the lumen of the ileum usually contains blood clots combined with fibrinonecrotic debris. Under a microscope, several changes in cell structures can be observed in affected areas of the intestinal mucosa. Ileitis causes enlarged crypts, in which the crypt epithelial cells develop irregular outlines that are often branched. The lack of goblet cells is also seen in intestines infected with L. intracellularis.
Microscopic changes in intestinum can be visualised by processing histological slides of intestinal tissue for immunohistochemistry (IHC) staining, which is also considered gold standard for confirmation of L. intracellularis presence in affected tissues. In addition, IHC can also be used to estimate the level of infection based on the amount of labeled L. intracellularis-specific antigen present in the intestinal mucosa. However, IHC requires specialised equipment and trained staff for analysis and proper interpretation, making this diagnostic method a costly one.
Detecting antibody presence
The humoral immune response starts 2 weeks after the pig is exposed to L. intracellularis. This is when L. intracellularis-specific antibodies in serum can be detected through serological assays such as immunoperoxidase monolayer assays (IPMA) and enzyme-linked immunosorbent assays (ELISA). There is a peak in the immune response at weeks 3 and 4, and the specific antibodies remain detectable up to 13 weeks post-infection.
Cross-sectional or longitudinal serological surveys every 3 weeks can then be an efficient approach to assess L. intracellularis circulation within the herd. When interpreting the serological results, other sources of antibodies than the humoral response to infection should also be taken into consideration, including the maternally derived antibodies that a piglet ingests with the colostrum. These type of antibodies remain present for up to 5 to 6 weeks of age. Antibodies can also be present as a response to prophylactic vaccination. Detectable serum antibodies can be expected when a dead vaccine is used. Pigs that orally receive a modified live vaccine rarely develop detectable titres of serum antibodies after contact with L. intracellularis.
Catching bacteria DNA parts
Amplification techniques, such as standard PCR and real-time (q)PCR, offer potentially rapid and sensitive ways to demonstrate the presence of L. intracellularis DNA (fractions) in faecal samples, rectal swabs or intestinal samples. Shedding can start 1 week post-infection. Consequently (q)PCR offers a more rapid and accurate ante-mortem detection of L. intracellularis during the first stages of infection. The presence of the bacteria does not necessarily indicate a negative impact on the pig’s health. However, researchers have demonstrated that L. intracellularis excretion correlates with the severity of lesions in histopathology and IHC of chronic cases, which in turn are associated with its clinical relevance.
For the subclinical form of the disease, the increasing number of L. intracellularis in faeces demonstrated a strong correlation with reduced daily gain and growth levels. In other words: the higher the bacterial load, the stronger the negative impact on swine health and performance. These results also underline the importance of understanding the limitations of detection and quantification of all used techniques implemented in analytical labs for appropriate diagnostics. In addition, keep in mind that molecular techniques are unable to differentiate pathogenic strains of L. intracellularis from the live attenuated vaccine strain.
Conclusion
L. intracellularis remains an important bacterial pathogen in pigs, but also a challenging one to diagnose. Coming to an accurate diagnosis is important to rule out other infections with similar gross presentations and to enable appropriate advice and interventions, in order to safeguard animal welfare and farm profitability. Different diagnosis methods can be used, each having their pros and cons.
However, by applying solid veterinary assessment on farm, in combination with proper sampling, macroscopic and microscopic assessment of lesions and advanced laboratory tools, veterinarians can reach an accurate and early diagnosis of the disease. In the upcoming parts of this article series, control and prevention of the disease will receive more attention.
References are available on request.
Read part 1: Lawsonia intracellularis: A challenging pathogen
 Beheer
Beheer




 WP Admin
WP Admin  Bewerk bericht
Bewerk bericht